The first ever UBT Co-Lead Peer-Learning event opened with SHARE Union organizer Janet Wilder thanking everyone in the room. Janet said that the newly defined relationship between SHARE members and managers is the most important language in our contract as we aim to improve the culture of our hospital. She explained that Unit-Based Teams are the cornerstone of that agreement, the most concrete and hopeful effort toward changing how it feels to work here.
Janet is the SHARE Tri-Chair of our Labor-Management Partnership Council, along with Bart Metzger, Chief Human Resources Officer, and Jeff Smith, Chief Operating Officer,
who also
kicked off the
meeting by talking about the importance of UBTs. Jeff Smith said that involving front-line staff in fixing the problem is better than the alternative: “I could give you an answer quickly, but it would be a bad solution.”

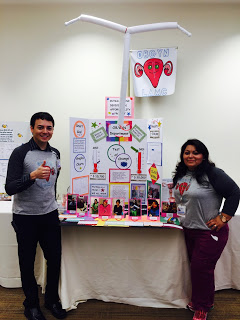
The first UBT Peer Learning Session brought together UBT Co-Sponsors and Co-Leads from SHARE, along with their management counterparts, as well as representatives from CITC, HR, and UMMC Executive Leadership. They came together to compare notes about the challenges and successes so far in the first wave of Unit Based Teams
As the hour developed, it became clear to everyone in the room that, across the board, the Unit-Based Teams are off to a productive and promising start. Each UBT has selected one or two substantial problems to tackle in their areas. They've defined their goals, and have begun measuring the effectiveness of their ideas.

SHARE Member and Lead Cardiac Catheterization Technologist, Sue Maddalena, describes how their UBT disregarded the advice that teams should avoid tackling the hardest problems first. They're seeing early successes as they work to improve the start times of their cases.
Each UBT explained very different situations, different approaches, and different results thus far, even between the two Prescription Centers involved, on both the University and Memorial campuses. Nonetheless, common trends appeared throughout. Communication in areas with UBT's has improved, sometimes considerably. That communication is helping the day-to-day work go more smoothly, and improving the work culture.

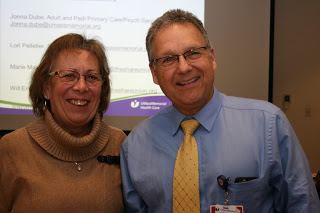
In Primary Care, they're kicking butt and collecting data. Where employees were previously frustrated with walk-ins, they're now opportunities to collect data to fix the problem. Rita Caputo (SHARE Co-President, pictured above left) tracks the progress of their system improvements.
SHARE member and Ambulatory Services Rep Mary Misiaszek said that, in her area, she had encountered one particularly meaningful new improvement: deeper respect. In addition, she said different parts of the clinic now "appreciate what everybody did, because we didn't know what everybody did before."
Mary noted, however, that one of the major challenges they faced was just understanding one another, since each kind of work in the hospital involves its own jargon and specialized language. As an ASR, her understanding of the distinction between words like "rapid" and "stat" differs from some co-workers, who use those words within the boundaries of defined clinical guidelines.
The hospital's
Center for Innovation and Transformational Change
often came up in the discussion, with participants noting the importance of the role of CITC in providing common language for discussing improvement.

SHARE member Kim Latrobe, a Technologist in the Surgical Vascular Lab, says that her co-workers are more willing to speak up about problems now, and more optimistic about the way that management will consider their ideas.
Some in the room commented that their department staff had found it meaningful to see SHARE and hospital leadership coming together around the Unit Based Teams. Although SHARE members have experienced many different initiatives aimed at improvement over the years, this feels different. Working through issues in a process where all participants have equal voice creates mutual accountability and improved chance of continual improvement.

Bart Metzger, UMass Memorial Senior Vice President and Chief Human Resources Officer, said that hospital CEO Eric Dickson increasingly references the importance of UBT's in meetings among hospital executives. Metzger describes the function of the UBTs toward the hospital's goals of transforming and humanizing our institution, and turning the traditional management paradigm on its head.
In the recent months, the participants in these first UBT's have learned a lot about how to launch a UBT successfully . . . much of it by trial-and-error. During the Peer Learning Session, many participants thanked the UBT Coaches and their own Co-Sponsors, who have been supporting the teams with tools and strategies for tackling big problems productively.
Although the UBT model involves a lot of planning, there have definitely been surprises in their initial experiments. The participants recommended even more training and more planning time, and encouraged the Coaches and Co-Sponsors to begin working with the next wave of UBT's as soon as possible, even though those teams won't be launching until after Epic Go-Live. We look forward to hearing more from this first group of UBT's.

SHARE Staff Organizers Janet Wilder and Will Erickson collect ideas and advice for improving the launch of the next wave of Unit Based Teams
The hour-long meeting brought together union members and management from the University Campus and the Memorial Campus, not to mention a labor-management pair who commuted in from our hospital's Tri-River facility in Uxbridge.
It wasn't easy to coordinate a time when so many could be away from their desks and workstations.
W
e know that whenever employees step away from the front lines to meet, it puts more pressure on those who remain in the departments to care for patients. We recognize those of you who are working in areas with UBT's for getting this important project started in such a strong way
. Already hundreds of SHARE members have helped move the work forward. Thank you.